Product Liability Update
Ten Things to Know About the New Unique Device Identifier Rule for Medical Devices
Many medical devices will soon carry a unique identity code, under a new rule recently published by the U.S. Food and Drug Administration (FDA). The FDA refers to this as the Unique Device Identifier (UDI) rule.
A medical device is a medical or health machine, implant, instrument or other similar article. It is intended for use in diagnosing, treating or preventing disease in humans or other animals. Medical devices act through physical, mechanical or thermal methods. This distinguishes them from pharmaceuticals and drugs, which act through chemical or metabolic methods. Some of the most common types of medical devices are artificial hips and knees, pacemakers, breast implants, coronary stents, artificial eye lenses and internal bone fixation hardware.
Here are 10 questions and answers about the new Unique Device Identifier rule for medical devices.
What is a Unique Device Identifier?
The incoming rule requires that medical devices, with limited exceptions, be labeled with a unique device identifier. The UDI is made of two parts: a device identifier and a production identifier. The device identifier is the version or model of the device. The production identifier identifies a specific device through a serial number, lot, batch, expiration date or manufacture date. The UDI must be placed on the medical device label and packaging.
What will a Unique Device Identifier look like?
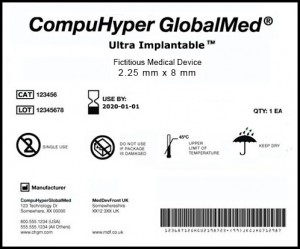
Here is a fictitious example of what a UDI would look like, according to the FDA’s website:
Most UDIs will not be directly marked onto devices, unlike some other kinds of stamped products like cars and tires. Because UDIs are supplied as part of the labeling and packing, it is likely that most will generally be given to medical providers and may not ultimately be passed on to patients. Devicemakers do not themselves create UDIs and instead must acquire them from accredited issuing agencies.
When will this happen?
The FDA’s phased-in approach focuses first on devices that pose the greatest risks. The UDI deadline for Class III devices is Sept. 24, 2014. Class III devices have the most stringent regulatory controls. They support or sustain human life, are of substantial importance in preventing impairment of human health, or present potential unreasonable risk of illness or injury. Examples of Class III devices are replacement heart valves, silicone breast implants, some prostheses, stents and extended wear contact lenses. By Sept. 24, 2015, class I and class II implantable, life-supporting and life-sustaining devices must bear a UDI. The FDA has published a specific list of devices that fall into this category. Devices that are intended for more than one use must be directly marked. By Sept. 24, 2016, all other class II devices must have a UDI. Class II devices have special controls that may include labels, performance standards or they may be monitored after sale. Class II devices include, for example, X-ray machines, powered wheelchairs, fixation devices, mesh, bone and vascular grafts, and surgical and acupuncture needles.
As the last phase, by Sept. 24, 2018, class I devices and unclassified devices must have a UDI. Class I devices pose minimal potential harm to the user and have a simple design. Examples are handheld surgical instruments, arm slings and splints, bandages and exam gloves.
What about devices that are already made?
Devices in inventory are exempt from UDI for another three years beyond their applicable compliance deadline. This means that manufacturers need not pull back devices in inventory for additional marking.
What kind of date format will be used?
The FDA adopted a global date format. The coding will use the standard format consistent with international practice, meaning year-month-day (i.e., 2013-11-30). This format avoids creating a special approach for the US and better ensures that dates are not confusing or misleading.
Are there any exceptions?
Very few. The following types of products are exempted from and do not need to have a UDI: custom devices, investigational devices, shipping containers, and class I devices that are exempt from the FDA’s 510(k) premarket notification and good manufacturing practice requirements.
How will the FDA track this new data?
The incoming rule also creates a new publicly searchable database. The FDA calls this the Global Unique Device Identification Database (GUDID, which the FDA suggests be pronounced “good id”). It will serve as a reference catalog for every device with an identifier.
Labelers must enter the device’s identifier in accordance with the compliance timetable. Production identifiers are not submitted to or stored in the GUDID. The public will have access to information in the database. The public database search function is not yet operational. The FDA states that it will be available after a meaningful dataset of device identifier records has been created.
This new database is similar to those that other federal agencies have run for years. The National Highway Traffic Safety Administration has a public database in which the public can search for information on recalls and complaints through searches such as keyword, model vehicle or model tire number. In 2011, the Consumer Product Safety Commission launched a publicly searchable database for reports of harm involving consumer products.
What about patient privacy issues?
Whenever data of a new type begins to be collected, stored and used, it is helpful to think through privacy issues. No identifying patient information will be stored in the new database. Patients’ medical records will include these codes, but medical records are already covered under the privacy rules of the Health Insurance Portability and Accountability Act.
How will this help detect repeating or common problems?
Even before the need for a recall is detected, “adverse event” reports may be made to the FDA. Those are reports of potential safety concerns that are made to the FDA by medical providers, patients or others. The new rule requires that UDIs be included in adverse event reports. That should allow manufacturers and the FDA to more quickly review, aggregate and analyze related reports about a specific device. That could lead to isolation and identification of a repeating problem, and could assist with development of a solution.
How will this affect recalls?
There have been 1,141 FDA recalls of medical devices so far in 2013, affecting 57.6 million units. The new rule should help with the speed and precision of recalls. Delays in identifying recalled devices can result in additional risk to patients. Recalls that go on for long periods of time also add costs for manufacturers and distributors in time and money. Medical devices that are implanted in the body and not capable of being immediately identified on sight can be especially challenging to quickly identify.
One of the benefits of a UDI is that a medical device can be identified rapidly and with great precision. This can result in recalls being conducted faster and with greater accuracy. As a similar example, through data tracking of the parts used in cars, General Motors Co. (GM) was recently able to pinpoint particular cars with a problematic valve. GM narrowed down the cars fitted with the part to only four cars, instead of potentially hundreds or thousands that it would otherwise have had to recall.
This represents the future of recalls.